Results
Since opening in 2019, Göteborgs IVF Klinik has been among the top clinics in Sweden in terms of pregnancies, ongoing pregnancies, and live births. From the very beginning, we have closely monitored our outcomes in every part of the process to give our patients the best possible chance of having a child through treatment with us. Some of the reasons for our high success rates are our experienced and well-informed staff, strong continuity (we do our best to ensure you meet the same doctor/midwife/nurse throughout your treatment), and that we use the very latest technology and equipment, including a new laboratory with state-of-the-art ventilation.
Göteborgs IVF Klinik – results among the best
Comparisons between Sweden’s IVF clinics
Outcomes from the majority of IVF clinics in Sweden are reported to Q-IVF, the national quality registry for IVF treatments. These results are typically published with about a two-year delay. During the pandemic, the lag was somewhat longer.
When comparing clinics, it is important—and common knowledge among gynecologists/IVF physicians—to relate the number of live births per embryo transfer to the expected number based on each clinic’s unique patient mix. Factors such as a woman’s age, prior IVF live births, and the number of previous treatment cycles all have a major impact on outcomes.
Our results
Between February 2020 (when the clinic opened) and February 2023, according to our own calculations, we achieved a live birth rate per egg retrieval (fresh transfer) of 24.4% for women up to 43 years of age. For frozen embryo transfers (FET) in women up to 45 (with oocytes retrieved by age 43), the live birth rate was 38.5%. These figures are not cumulative and show that Göteborgs IVF Klinik ranks among the top nationally.
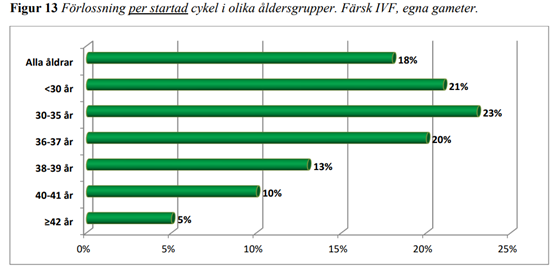
For comparison, see the figure below taken from Q-IVF’s public outcome report. It is based on data from all IVF clinics in Sweden and shows results broken down by age groups, since pregnancy chances are primarily influenced by the woman’s age.
Please note that results can be affected by differences in patient populations between clinics, for example the average age within the listed age categories.
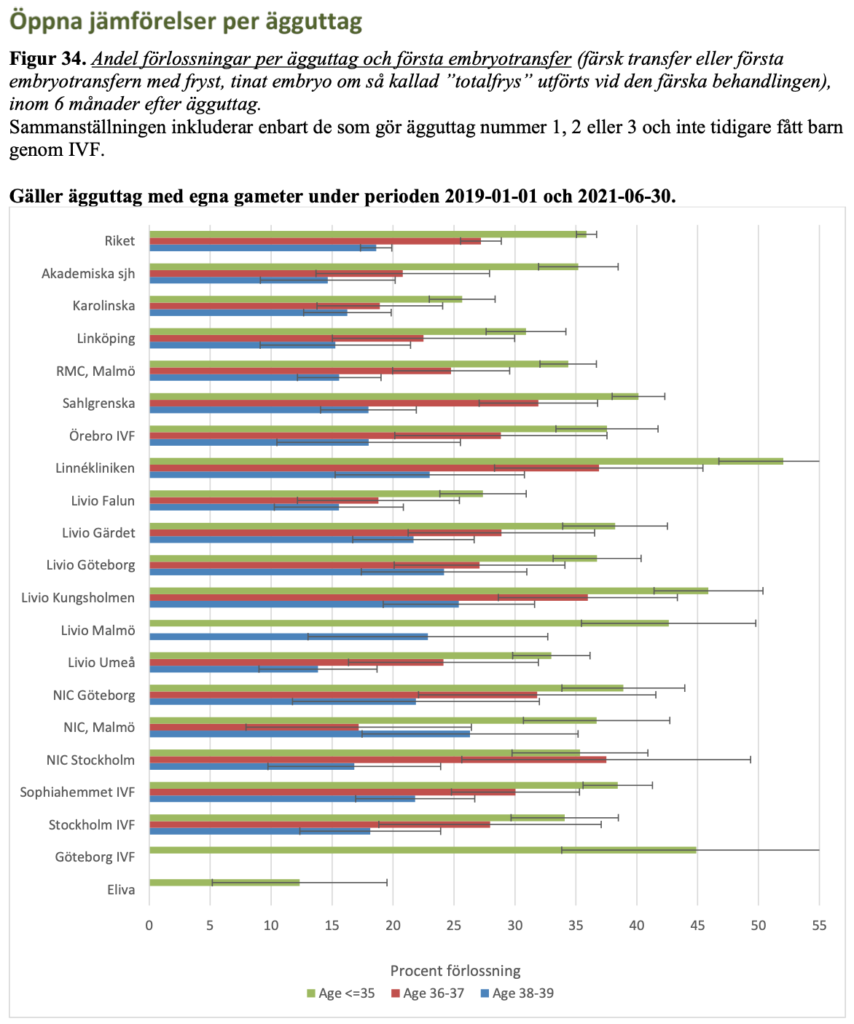
For more information, please visit the Q-IVF website where all results are intended to be publicly available under EU legislation. There too it is clear that Göteborgs IVF Klinik’s outcomes are among the best in Sweden.
In Q-IVF, results are often presented by age groups because pregnancy chances largely depend on the woman’s age. In the figure below, concerning open comparisons, only results for women undergoing IVF up to and including age 39 are shown. Note that the results may be somewhat misleading because some clinics treated couples with a higher average age within each age group.
Why choose us?
Many patients wonder which IVF clinic to choose for their treatment. The image below summarizes why we can confidently recommend choosing us. Support for each point can be found on this page and throughout our website.
- Best outcomes (national comparison adjusted for expected results)
- Best patient care (national comparison)
- Lowest prices among clinics in Gothenburg
- Short waiting times – first consultation within 1–2 weeks; you can start treatment with your next period (provided the evaluation is complete)
- Central Gothenburg location with ample parking around the clinic
- If you need accommodation, we collaborate with Hotel Jazys and can offer a discounted rate
- Private patient rooms for egg retrieval and embryo transfer
Strong results in KUPP
KUPP 2024
KUPP 2023
KUPP 2022
General points when reviewing results
When results are reviewed, it’s important to note that figures can vary significantly depending on whether outcomes are reported per embryo transfer or per initiated treatment. In addition, some treatments are discontinued shortly after stimulation begins for various reasons, or embryo transfer cannot be performed because there are no embryos of sufficient quality for transfer.
Another common reason for not performing a fresh transfer is when all embryos that meet freezing criteria are frozen due to the risk of ovarian hyperstimulation (OHSS). This means fewer patients complete a treatment than start one. The proportion of pregnancies per embryo transfer therefore becomes higher compared with outcomes per initiated treatment or per oocyte retrieval. Results must also be reviewed today with respect to whether the transfer is fresh or frozen.
This is because frozen embryos are now mainly blastocysts, which have a much higher chance of pregnancy (see below). Furthermore, results from fresh transfers must be divided into day-2/3 transfers versus blastocyst transfers for the same reason.
What determines whether IVF treatment succeeds?
The single most important factor is the woman’s age. Natural fertility has already declined markedly by age 36–37 compared with age 20. The same age effect is seen in IVF outcomes. With increasing age, the number of oocytes declines and egg quality worsens, leading to fewer pregnancies and more miscarriages.
Therefore, we apply an age limit of 43 years for the woman, as treatments above that age result in very few pregnancies according to many studies.
Even though age is the most important factor for success, there is considerable variation between women in the ages where results start to fall. Each woman’s prerequisites differ, so we perform an individual assessment and provide individualized advice. This includes a careful examination of the ovaries by ultrasound and blood hormone tests taken before treatment.
During ultrasound, we count the number of antral follicles (estimate ovarian reserve) and assess ovarian size. Pregnancy chances are higher the more antral follicles there are (and the larger the ovaries are). Thus, a 39–40-year-old with a “good” ovarian reserve may have a similar chance of success as a clearly younger woman with a much lower reserve.
However, a young woman with a very low reserve still has a much higher chance of becoming pregnant than an older woman with the same low reserve. This assessment/advice is given at the first doctor’s visit.
The blood tests that complement the ultrasound are AMH (anti-Müllerian hormone) and, if needed, FSH (a pituitary hormone). AMH in particular is a good indicator of remaining oocytes (ovarian reserve) and thus the patient’s chance of success.
Transferring one or two embryos
We follow the Swedish National Board of Health and Welfare’s directive to transfer a single embryo in most cases to reduce twin pregnancies. Previously (before ~2000–2005), two embryos were often transferred. The rationale for recommending a single-embryo transfer (ET) is that studies have shown a clearly increased risk for children born as twins compared with singletons. For example, the risk of cerebral palsy in twins is about four times higher than in singletons.
(Risk figures for twins conceived through IVF do not differ from those for twins conceived without IVF.)
A large multicenter study published in 2005 showed that the chance of becoming pregnant/having a baby after one oocyte retrieval—including any frozen-thawed transfers from the same cycle—was the same as when two embryos were transferred at once after the same retrieval. In other words, outcomes remained at the high level we were accustomed to when two embryos were routinely transferred.
This happened while Sweden reduced the twin delivery rate to just over 2% (down from about 28%). Most importantly, prioritizing single-embryo transfer has resulted in healthier children and a dramatic 70% reduction in babies with, among other things, low birth weight (a key risk factor for cerebral palsy). Perinatal mortality has also fallen by about 70%.
Today, the risks of low birth weight and perinatal death in IVF are at the same level as in spontaneously conceived pregnancies. At Gothenburg IVF Clinic, our twin rate is 1.5%, which is excellent.
Transfer on day 2 or 3, or as a blastocyst
Blastocyst culture—growing an embryo longer, often to day 5 (sometimes day 4 or 6)—is used to select the best embryo to transfer with the highest chance of pregnancy. Ideally, an embryo develops into a blastocyst containing around 150–200 cells. During extended culture, some embryos arrest or fail to develop, and only those with the best potential remain.
One reason is that not all embryos are of high quality, and the longer culture allows us to see which have better versus poorer potential.
If the woman/couple has fewer than five fertilized oocytes, we generally choose the shorter two- or three-day culture. If there are many fertilized oocytes—which is common—we extend to blastocyst culture to help select which embryo to transfer. We achieve very good results with both transfer strategies.
Complications in IVF
The complication risk in IVF in Sweden today is very low, and IVF is considered a very safe method for both mother and baby. The largest risk is OHSS (ovarian hyperstimulation syndrome). Most clinics in Sweden report 1–2% OHSS (1–2% of treated women) and around 0.3% infection rates on average. Other less common complications for the woman can include bleeding and blood clots.
At Gothenburg IVF Clinic, our OHSS rate is below 0.1% (despite having an unusually high proportion of patients with PCOS, a risk factor for OHSS), and infection is also below 0.1% (based on more than 800 oocyte retrievals).
With us, you can feel very safe while benefiting from some of Sweden’s best IVF outcomes according to Q-IVF calculations—together with good prices, excellent patient care and short waiting times for treatment. A warm welcome to our clinic!


